TIA: The Silent Warning Before A Stroke Strikes
A Transient Ischemic Attack (TIA), often referred to as a "mini-stroke," is a critical medical event that demands immediate attention. While its symptoms are fleeting and cause no permanent damage, a TIA serves as a powerful and urgent warning sign that a full-blown stroke could be imminent. Understanding what a TIA is, recognizing its symptoms, and knowing how to respond can be the difference between a temporary scare and a life-altering medical emergency.
This comprehensive guide will delve into the intricacies of Transient Ischemic Attacks, exploring their causes, symptoms, and the crucial steps you should take if you suspect you or someone you know is experiencing one. We will emphasize why a prompt medical evaluation is not just recommended, but absolutely vital for preventing future, more severe cerebrovascular events. By the end of this article, you will have a clearer understanding of this often-misunderstood condition and be empowered with the knowledge to protect your brain health.
Table of Contents:
- Understanding Transient Ischemic Attack (TIA): A Brief Overview
- The Critical Link Between TIA and Stroke Risk
- Recognizing the Symptoms of a Transient Ischemic Attack
- Causes of TIA: What Blocks Blood Flow to the Brain?
- The Urgency of Prompt Evaluation and Diagnosis
- Treatment and Management Strategies for TIA
- Living Beyond a TIA: Prevention and Long-Term Health
- Differentiating TIA from Other Neurological Conditions
Understanding Transient Ischemic Attack (TIA): A Brief Overview
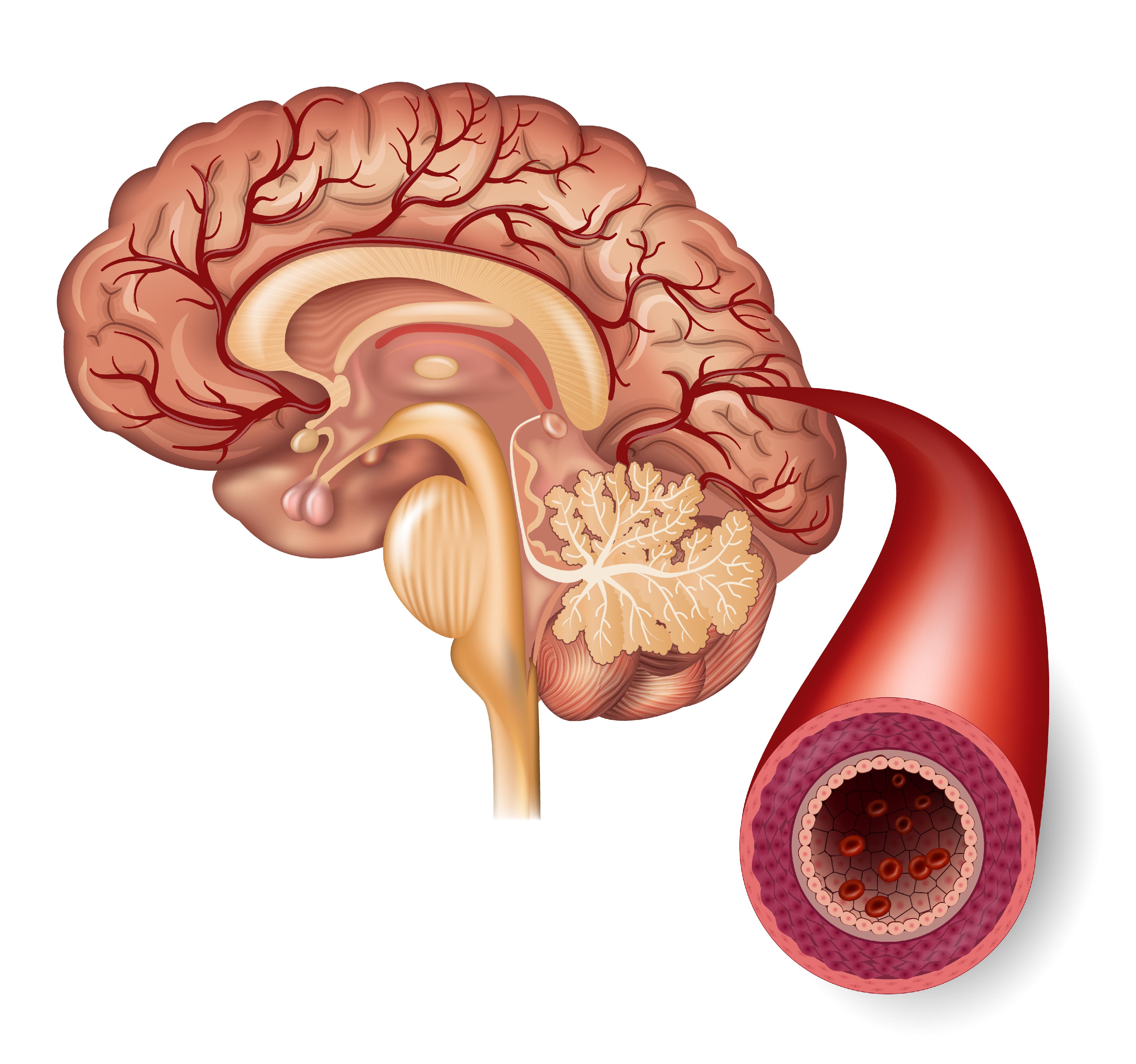
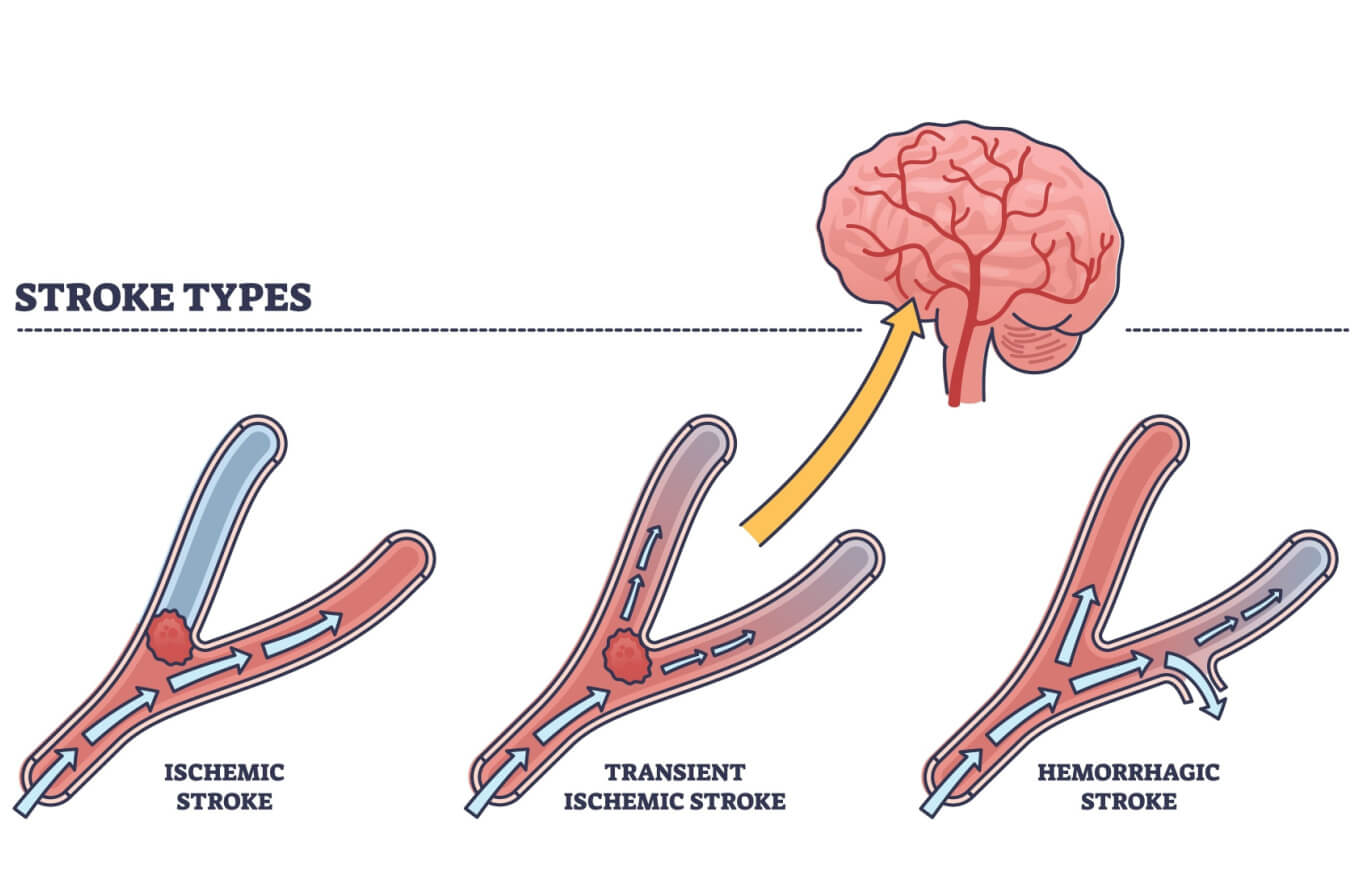
A Transient Ischemic Attack (TIA) is a neurological event characterized by symptoms similar to those of a stroke, but which last for a very short period, typically only a few minutes, and rarely more than 24 hours. The defining characteristic of a TIA is that it does not cause permanent brain damage, unlike a full stroke. This temporary disruption of brain function occurs due to a brief blockage of blood flow to the brain. Imagine a temporary kink in a garden hose; the water flow stops for a moment, but then quickly resumes without lasting damage to the plants. In the brain, this temporary blockage means that a part of the brain is deprived of oxygen and nutrients for a short time, leading to the transient symptoms. Because the blockage is brief and the blood flow is restored quickly, the brain cells do not die, which is why there is no permanent damage. However, this fleeting nature should not lead to complacency; rather, it should heighten concern. It’s a clear signal that something is amiss within the brain's vascular system, and it demands immediate investigation.
The Critical Link Between TIA and Stroke Risk
Despite its transient nature and lack of permanent damage, a Transient Ischemic Attack is far from benign. In fact, it is one of the most significant warning signs that a person is at high risk of experiencing a full-blown stroke in the near future. Think of a TIA as a "dress rehearsal" for a stroke, or perhaps a flickering warning light on your car's dashboard. It indicates an underlying problem that, if left unaddressed, could lead to a much more severe and permanent event. Statistics underscore this critical link: approximately 1 in 3 people who experience a TIA will go on to have a stroke. A significant portion of these strokes occur within days or weeks of the TIA. This alarming statistic highlights why immediate medical attention after a TIA is not just advisable, but absolutely crucial for stroke prevention. The symptoms may pass, but the underlying risk remains, often increasing in the days and weeks following the TIA. Ignoring a TIA is akin to ignoring a smoke detector; while there might not be a fire yet, the warning is undeniable.
Recognizing the Symptoms of a Transient Ischemic Attack
The symptoms of a Transient Ischemic Attack are identical to those of a stroke because they both stem from a disruption of blood flow to the brain. The key difference lies in their duration. TIA symptoms come on suddenly and typically resolve within minutes. However, even if symptoms disappear quickly, they should never be dismissed. The acronym FAST is often used to help people remember the common signs of a stroke or TIA:
- F - Face Drooping: One side of the face may droop or feel numb. Ask the person to smile. Is the smile uneven?
- A - Arm Weakness: One arm may feel weak or numb. Ask the person to raise both arms. Does one arm drift downward?
- S - Speech Difficulty: Speech may be slurred, or the person may have trouble speaking or understanding speech (aphasia). Ask the person to repeat a simple sentence. Is it difficult or garbled? Sometimes, temporary episodes of aphasia can occur due to a TIA.
- T - Time to Call Emergency Services: If you observe any of these signs, even if they seem to improve, call for emergency medical help immediately.
Other potential symptoms of a Transient Ischemic Attack can include:
- Sudden weakness or numbness on one side of the body.
- Sudden confusion or trouble understanding.
- Sudden trouble seeing in one or both eyes.
- Sudden trouble walking, dizziness, loss of balance, or coordination.
- Sudden severe headache with no known cause.
Causes of TIA: What Blocks Blood Flow to the Brain?
A Transient Ischemic Attack occurs when there is a temporary decrease in blood supply to a part of the brain. This decrease is most commonly caused by a brief blockage of a blood vessel that supplies the brain. The primary culprits behind these blockages are often related to underlying cardiovascular conditions. Here are the main causes:
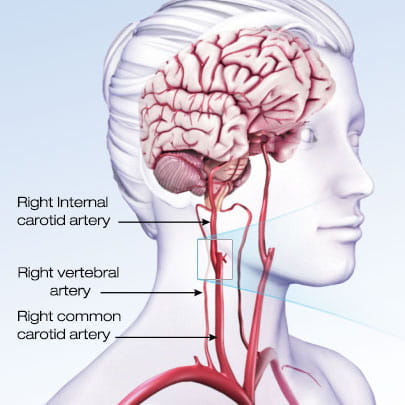
- Atherosclerosis: This is the most common cause. Atherosclerosis involves the hardening and narrowing of arteries due to the buildup of plaque (fatty deposits, cholesterol, cellular waste products, calcium, and fibrin) on their inner walls. When this plaque builds up in the carotid arteries (the major arteries in the neck that supply blood to the brain) or other arteries leading to the brain, it can significantly restrict blood flow. Carotid artery disease often develops slowly, and a TIA might be the very first sign of the condition.
- Blood Clots: A blood clot (thrombus) can form in an artery narrowed by atherosclerosis. Alternatively, a clot can break away from another part of the body (embolus), such as the heart (especially in conditions like atrial fibrillation, an irregular heartbeat), and travel through the bloodstream until it gets lodged in a smaller artery in the brain, temporarily blocking blood flow.
- Small Vessel Disease: This involves damage to the tiny blood vessels deep within the brain. While less common as a direct cause of TIA, it can contribute to overall brain health issues and increase stroke risk.
- Other Less Common Causes: These can include inflammatory conditions of blood vessels (vasculitis), certain blood disorders, or even a spasm of a blood vessel.
Understanding these causes is crucial because identifying the specific reason behind a TIA is the first step toward preventing a future, potentially devastating, stroke. The temporary shortage of blood flow to the brain, no matter how brief, is a direct result of one of these underlying vascular issues.
The Urgency of Prompt Evaluation and Diagnosis
The moment TIA symptoms appear, even if they resolve quickly, it is imperative to seek immediate medical attention. A prompt evaluation of your symptoms is vital to diagnose the cause of a Transient Ischemic Attack and to determine the best treatment plan to prevent a future stroke. This is a medical emergency, and acting quickly can save your life or prevent severe disability. Do not wait for symptoms to worsen, and do not assume they will simply go away and not return. Many people make the mistake of dismissing a TIA because the symptoms are temporary, but this is a dangerous oversight.
When you arrive at the emergency room, healthcare professionals will conduct a thorough examination. This often includes:
- Neurological Examination: To assess brain function, reflexes, and coordination.
- Imaging Tests:
- CT Scan or MRI of the Brain: To check for signs of a stroke, bleeding, or other brain abnormalities.
- Carotid Ultrasound: To look for narrowing or blockages in the carotid arteries in the neck.
- CT Angiography (CTA) or MR Angiography (MRA): To visualize blood vessels in the brain and neck.
- Heart Tests:
- Electrocardiogram (ECG): To check for heart rhythm problems like atrial fibrillation.
- Echocardiogram: To look for blood clots in the heart or other heart conditions.
- Blood Tests: To check cholesterol levels, blood sugar, and other factors that can increase stroke risk.
Institutions like Mayo Clinic, with their doctors trained in blood vessel and brain conditions (cerebrovascular specialists), emphasize a rapid and comprehensive approach to Transient Ischemic Attack care. Their care teams are equipped to quickly diagnose the underlying cause and implement preventative strategies. This swift action is critical because the risk of a full stroke is highest in the hours and days immediately following a TIA. The goal is not just to confirm a TIA, but to identify *why* it happened and to intervene before a more severe event occurs. Remember, a TIA is a warning signal; responding to it promptly is your best defense against a future stroke.
Treatment and Management Strategies for TIA
The primary goal of Transient Ischemic Attack treatment is to prevent a future stroke. Once the cause of the TIA has been identified, your healthcare professional will determine the most appropriate course of action. Treatment strategies often involve a combination of medication, lifestyle changes, and, in some cases, medical procedures.
Medication:
- Antiplatelet Drugs: These medications, such as aspirin or clopidogrel (Plavix), help prevent blood clots from forming. They work by making platelets, tiny blood cells, less sticky and less likely to clump together. If the cause of the TIA is a narrowed blood vessel in the head, these are often recommended.
- Anticoagulants: For individuals with certain heart conditions like atrial fibrillation, stronger blood thinners (anticoagulants) may be prescribed to prevent blood clots from forming in the heart and traveling to the brain.
- Cholesterol-Lowering Drugs (Statins): If high cholesterol is a contributing factor to atherosclerosis, statins are prescribed to reduce plaque buildup in the arteries.
- Blood Pressure Medications: High blood pressure is a major risk factor for TIA and stroke. Medications to control blood pressure are often a cornerstone of treatment.
- Cilostazol: In cases where large arteries are severely blocked, cilostazol may be prescribed in addition to aspirin or clopidogrel to improve blood flow.
Lifestyle Changes:
Modifying lifestyle factors is crucial for reducing stroke risk:
- Healthy Diet: Emphasize fruits, vegetables, whole grains, and lean proteins while limiting saturated and trans fats, cholesterol, and sodium.
- Regular Exercise: Aim for at least 150 minutes of moderate-intensity aerobic activity per week.
- Smoking Cessation: Smoking significantly increases stroke risk and should be stopped immediately.
- Moderate Alcohol Consumption: Limit alcohol intake.
- Weight Management: Maintain a healthy weight to reduce strain on the cardiovascular system.
- Diabetes Management: If you have diabetes, strict control of blood sugar levels is essential.
Procedures:
In some cases, if a TIA is caused by severe narrowing of a major artery, particularly the carotid artery, a medical procedure may be recommended:
- Carotid Endarterectomy: A surgical procedure to remove plaque buildup from the carotid artery in the neck.
- Carotid Angioplasty and Stenting: A less invasive procedure where a balloon is used to widen a narrowed artery, and a stent (a small mesh tube) is inserted to keep it open.
The specific treatment plan will be tailored to the individual's unique circumstances, underlying causes, and overall health. Adhering to this plan diligently is paramount for preventing a future, potentially debilitating, stroke.
Living Beyond a TIA: Prevention and Long-Term Health
Experiencing a Transient Ischemic Attack is a wake-up call, a clear signal that proactive steps are needed to protect your long-term health and prevent a stroke. Living beyond a TIA means committing to ongoing risk management and adopting a heart-healthy and brain-healthy lifestyle. It’s not just about taking prescribed medications; it’s about a holistic approach to wellness that addresses the root causes of the TIA.
Key aspects of long-term prevention include:
- Consistent Medication Adherence: This is non-negotiable. Whether it's antiplatelet drugs, blood pressure medication, or cholesterol-lowering drugs, taking them exactly as prescribed is vital. Do not stop or alter your medication without consulting your doctor.
- Aggressive Management of Risk Factors:
- Blood Pressure Control: Regularly monitor your blood pressure and work with your doctor to keep it within target ranges.
- Cholesterol Management: Follow dietary recommendations and take prescribed medications to keep cholesterol levels healthy.
- Diabetes Control: If you have diabetes, meticulous management of blood sugar levels is crucial, as uncontrolled diabetes significantly increases stroke risk.
- Smoking Cessation: If you smoke, quitting is the single most impactful step you can take.
- Regular Physical Activity: Incorporate regular exercise into your routine to improve cardiovascular health.
- Healthy Diet: Maintain a balanced diet rich in fruits, vegetables, and whole grains, and low in processed foods, saturated fats, and sodium.
- Weight Management: Achieve and maintain a healthy weight.
- Regular Medical Check-ups: Schedule follow-up appointments with your healthcare team to monitor your condition, adjust medications if necessary, and assess your overall cardiovascular health. These check-ups are essential for ongoing risk assessment and prevention.
- Stress Management: Chronic stress can contribute to high blood pressure and other risk factors. Explore stress-reducing techniques like meditation, yoga, or hobbies.
- Education and Awareness: Continue to educate yourself about stroke symptoms and risk factors. Share this knowledge with family and friends so they can also be prepared to act quickly if needed.
A TIA offers a unique opportunity for intervention. By taking these steps seriously, individuals can significantly reduce their risk of a future stroke and enjoy a healthier, more fulfilling life. It's a journey of continuous vigilance and commitment to well-being.
Differentiating TIA from Other Neurological Conditions
While the symptoms of a Transient Ischemic Attack are distinct, they can sometimes overlap with those of other neurological conditions. Accurate diagnosis is crucial to ensure appropriate treatment and prevention strategies. Understanding the nuances between TIA and other conditions is key.
TIA vs. Stroke: Key Distinctions
The most important distinction between a TIA and a stroke lies in the outcome. A stroke (ischemic stroke) results in permanent brain damage due to prolonged interruption of blood flow, leading to lasting neurological deficits. A TIA, on the other hand, involves a brief blockage of blood flow that resolves before permanent damage occurs. The symptoms are identical, but their duration and the presence of permanent damage differentiate them. If symptoms persist for more than a few minutes, or if there are any lingering deficits, it is more likely a stroke, even if it's a small one. However, it's impossible to tell the difference without medical evaluation, which is why both warrant immediate emergency care.
Migraines and Seizures: Similarities and Differences
Sometimes, temporary episodes of neurological symptoms, such as aphasia (difficulty with speech), can occur due to migraines or seizures, leading to confusion with a TIA.
- Migraine with Aura: Some migraines are preceded by an "aura," which can involve visual disturbances, numbness, tingling, or even speech difficulties. These symptoms typically develop gradually over 5-20 minutes and last less than an hour, often followed by a headache. TIA symptoms, by contrast, are usually sudden in onset.
- Seizures: Seizures are caused by abnormal electrical activity in the brain. Symptoms vary widely depending on the part of the brain affected, but can include sudden jerking movements, loss of consciousness, confusion, or temporary speech problems. While some seizure symptoms can mimic TIA, the presence of uncontrolled movements, post-seizure confusion (postictal state), or a history of epilepsy can help differentiate them.
Vascular Dementia and TIA's Role
Vascular dementia is a type of dementia caused by conditions that block or reduce blood flow to the brain, depriving brain cells of vital oxygen and nutrients. Symptoms vary depending on the part of your brain where blood flow is impaired and often overlap with those of other types of dementia, especially Alzheimer's disease. While a single TIA doesn't cause permanent damage, a history of multiple TIAs or small, silent strokes (often undetected) can contribute to vascular dementia over time. Each event, even if transient, can incrementally damage brain tissue, leading to cognitive decline. Therefore, preventing TIAs and strokes is also crucial for maintaining long-term cognitive health.
Other Vascular Conditions: Aneurysms and Malformations
While TIAs are caused by blockages, other serious cerebrovascular conditions involve structural abnormalities of blood vessels. These include:
- Arteriovenous Malformation (AVM): An abnormal tangle of blood vessels connecting arteries and veins in the brain, bypassing capillaries. AVMs can rupture and cause bleeding (hemorrhagic stroke) or put pressure on brain tissue.
- Brain Aneurysm: A bulge or ballooning in a blood vessel in the brain. Aneurysms are often asymptomatic until they rupture, leading to a subarachnoid hemorrhage, a life-threatening type of stroke.
- Carotid Artery Disease: As mentioned earlier, this is a major cause of TIA and ischemic stroke, involving narrowing of the carotid arteries due to plaque buildup.
- Dural Venous Malformation (DVM): Similar to AVMs but involving the dural veins, which can also lead to bleeding or other neurological issues.
Understanding these distinctions is crucial for healthcare professionals, but for the general public, the message remains clear: any sudden onset of stroke-like symptoms requires immediate medical attention. Let the experts determine the exact cause; your role is to act swiftly.
In conclusion, a Transient Ischemic Attack (TIA) is a powerful and unmistakable warning sign that your brain's blood supply is compromised, putting you at significant risk of a full-blown stroke. While its symptoms are temporary and cause no permanent damage, the underlying cause demands immediate and thorough medical evaluation. Ignoring a TIA is akin to playing Russian roulette with your brain health.
By understanding the symptoms, recognizing the urgency of prompt medical care, and committing to the recommended treatment and lifestyle changes, you can dramatically reduce your risk of a future, more severe cerebrovascular event. Remember the FAST acronym, and if you or someone you know experiences any stroke-like symptoms, even if they quickly resolve, do not hesitate to call emergency services immediately. Your swift action could be the key to preventing a life-altering stroke.
Has this article shed new light on the importance of TIAs for you? Share your thoughts or questions in the comments below. If you found this information valuable, please consider sharing it with others who might benefit. For more insights into brain health and stroke prevention, explore other articles on our site.
Mini Stroke Symptoms Tia Transient Ischemic Attack Sy - vrogue.co
Transient Ischemic Attack (TIA) | American Stroke Association
What Is A TIA (Transient Ischemic Attack) And How Can It, 50% OFF