NASH: Unveiling The Silent Threat To Your Liver Health
NASH (Nonalcoholic Steatohepatitis) is a progressive and often silent liver condition that has become a significant global health concern. Formerly known as nonalcoholic steatohepatitis, it represents a more severe form of fatty liver disease, where the accumulation of fat in the liver is accompanied by inflammation and damage to liver cells. This progression can lead to serious complications, making early understanding and intervention crucial for maintaining liver health.
For many, the term "fatty liver" might sound benign, but the reality of NASH is far from it. It's a condition that can quietly advance, often without noticeable symptoms in its early stages, yet it carries the potential for severe consequences, including cirrhosis, liver failure, and even liver cancer. This article aims to demystify NASH, exploring its origins, risk factors, diagnostic approaches, and the vital strategies for its management, empowering you with the knowledge to protect one of your body's most essential organs.
Table of Contents
- Understanding NASH: A Progressive Liver Disease
- From NAFLD to NASH: The Spectrum of Fatty Liver Disease
- The Silent Progression: Why NASH is a Serious Concern
- Risk Factors for NASH: Unraveling the Metabolic Connection
- Diagnosing NASH: Beyond the Initial Suspicions
- Managing NASH: Lifestyle as the First Line of Defense
- NASH in Different Age Groups: Children and Adults
- Looking Ahead: Research, Treatments, and Hope for NASH Patients
Understanding NASH: A Progressive Liver Disease
The landscape of liver diseases has seen a significant shift, with conditions related to metabolic dysfunction becoming increasingly prevalent. Among these, NASH (Nonalcoholic Steatohepatitis) stands out as a particularly concerning form of liver damage. Historically, this condition was indeed referred to as nonalcoholic steatohepatitis, a term that accurately describes its core pathology: inflammation of the liver (hepatitis) not caused by alcohol, but by the accumulation of fat (steatosis). Today, it's often grouped under the broader umbrella of Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD), with NASH specifically being the inflammatory and damaging subtype, now known as MASH (Metabolic Dysfunction-Associated Steatohepatitis).
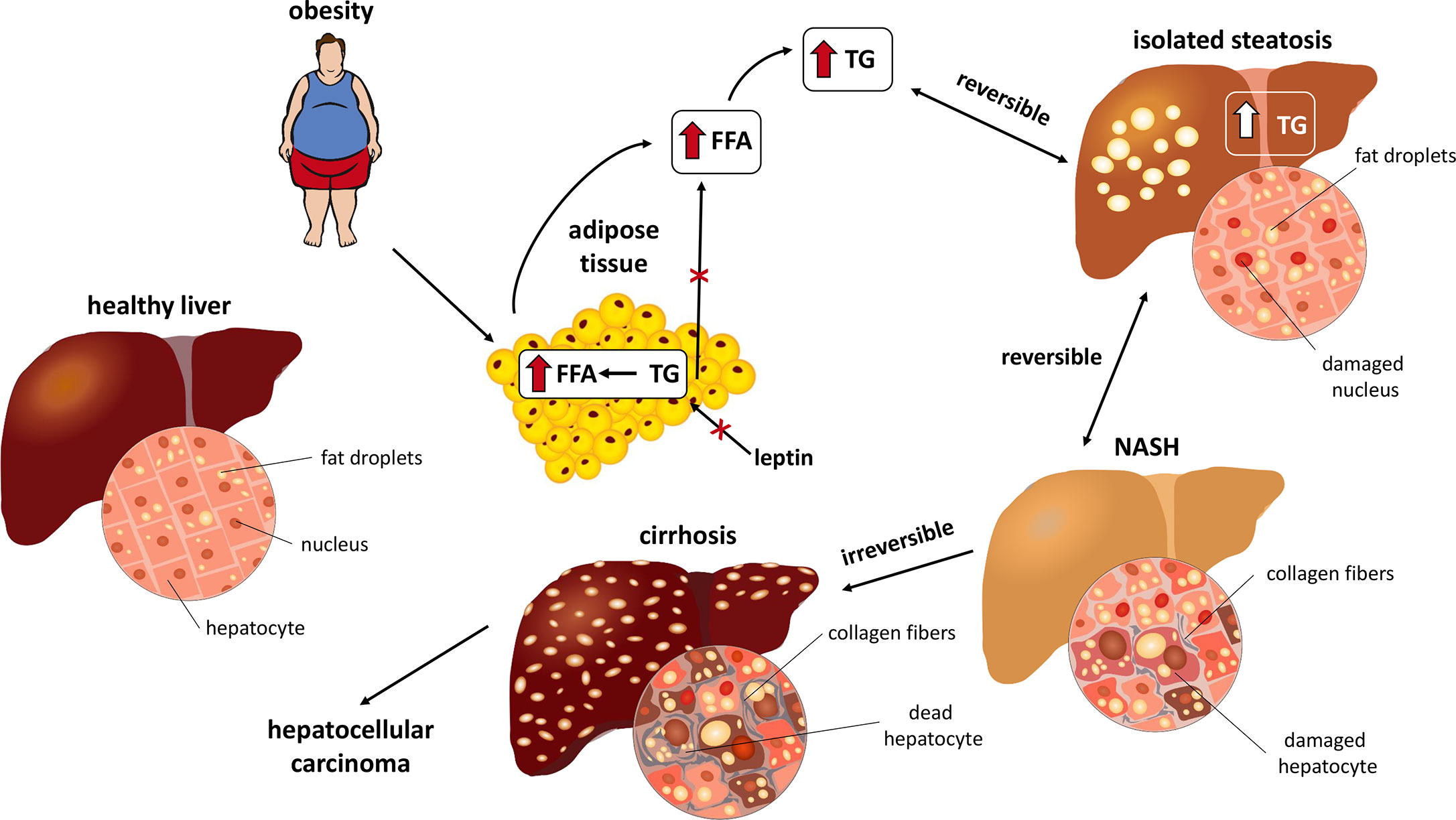
At its heart, NASH is a dangerous, progressive fatty liver disease where individuals experience liver inflammation and damage due to excessive fat accumulation, a process known as steatosis. This isn't just about having some fat in the liver; it's about that fat triggering an inflammatory response that actively harms liver cells. Unlike simple fatty liver (steatosis), which may not cause significant long-term damage, NASH involves cellular injury, ballooning degeneration of hepatocytes (liver cells), and often, fibrosis (scarring). This distinction is critical because the presence of inflammation and damage signifies a much higher risk of disease progression to more severe stages, ultimately impacting liver function and overall health.
The liver is an incredibly resilient organ, capable of regeneration and performing hundreds of vital functions, from detoxification to metabolism. However, persistent inflammation and damage, as seen in NASH, can overwhelm its regenerative capacity. Over time, this chronic injury can lead to the buildup of scar tissue, a process called fibrosis. If left unchecked, fibrosis can advance to cirrhosis, a severe form of scarring that permanently impairs liver function and significantly increases the risk of liver failure and hepatocellular carcinoma (liver cancer). Understanding NASH means recognizing it not just as a condition of fat in the liver, but as a dynamic and potentially devastating disease process that demands attention and proactive management.
From NAFLD to NASH: The Spectrum of Fatty Liver Disease
To fully grasp the significance of NASH, it's essential to understand its place within the broader spectrum of nonalcoholic fatty liver disease. These diseases were formerly called nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH). The recent reclassification reflects a deeper understanding of the underlying metabolic drivers, leading to the new terminology: Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD) encompassing the entire spectrum, and Metabolic Dysfunction-Associated Steatohepatitis (MASH) specifically for the inflammatory form.
The journey often begins with simple steatosis, where the liver accumulates fat but without significant inflammation or damage. If the tissue shows fat without inflammation, it falls under this category, which is generally considered less severe. Many individuals can live with simple fatty liver without experiencing major health complications, provided the condition doesn't progress. However, for a significant percentage of these individuals, the condition can worsen. This progression occurs when the accumulated fat begins to trigger an inflammatory response within the liver. This is the critical juncture where NAFLD transitions into NASH.
NASH is diagnosed when examination of the tissue with a microscope shows fat along with inflammation and damage to liver cells. This microscopic evidence of inflammation and hepatocyte injury (ballooning degeneration) is what differentiates NASH from simple fatty liver. It signifies that the liver is actively being harmed, setting the stage for fibrosis and potentially more advanced liver disease. The presence of inflammation accelerates the scarring process, which is why NASH carries a much higher risk of progressing to cirrhosis, liver failure, and liver cancer compared to simple steatosis. Understanding this spectrum is vital for both clinicians and patients, as it guides diagnostic strategies and treatment priorities, emphasizing the need for vigilance when inflammation and damage are detected.
The Silent Progression: Why NASH is a Serious Concern
The insidious nature of NASH lies in its "silent progression." For many years, individuals with NASH may experience no symptoms at all, or only very vague, non-specific complaints like fatigue or dull abdominal discomfort. This lack of clear warning signs means that the disease can advance significantly, sometimes to irreversible stages, before it is even detected. This silent march towards potential liver failure is precisely why NASH is considered a severe and concerning health issue.
The liver, with its remarkable regenerative capabilities, can compensate for damage for a long time. This compensatory mechanism, while beneficial in the short term, can mask the ongoing injury from NASH. Patients might feel perfectly healthy even as inflammation and scarring accumulate. By the time symptoms become apparent – such as jaundice (yellowing of the skin or eyes), ascites (fluid buildup in the abdomen), or confusion – the disease has often progressed to advanced fibrosis or cirrhosis. At this stage, the liver's ability to function is severely compromised, and the risk of life-threatening complications like liver failure or hepatocellular carcinoma (liver cancer) dramatically increases.
The severity of NASH also stems from its potential to accelerate other health problems. It's not just a liver disease in isolation; it's intricately linked to systemic metabolic dysfunction. Individuals with NASH often have an increased risk of cardiovascular disease, type 2 diabetes, and chronic kidney disease, further compounding their health burden. The silent progression of NASH underscores the critical need for awareness, proactive screening in at-risk populations, and early intervention strategies. Recognizing the potential for severe outcomes, even in the absence of overt symptoms, is key to mitigating its long-term impact and preventing the devastating consequences of advanced liver disease.
Risk Factors for NASH: Unraveling the Metabolic Connection
Understanding the risk factors for NASH is paramount for prevention and early detection. The primary drivers of NASH are deeply rooted in metabolic dysfunction, reflecting a global health crisis characterized by rising rates of obesity, type 2 diabetes, and related conditions. As medical experts continue to unravel the complexities of NASH, it becomes increasingly clear that it is often a manifestation of underlying metabolic imbalances within the body. Discover the main risk factors for NAFLD and NASH, including obesity, diabetes, and more, as highlighted by numerous studies and clinical observations.
Obesity and Type 2 Diabetes: Primary Drivers
At the forefront of NASH risk factors are obesity and type 2 diabetes. The global obesity epidemic has directly correlated with a surge in NASH cases. Excess body fat, particularly visceral fat (fat around organs), leads to increased inflammation and insulin resistance throughout the body, including the liver. Insulin resistance means that the body's cells don't respond effectively to insulin, leading to higher blood sugar levels and increased fat storage in the liver. This creates a vicious cycle where fat accumulation promotes inflammation, and inflammation exacerbates insulin resistance.
Type 2 diabetes is another powerful predictor of NASH. The chronic high blood sugar and insulin resistance characteristic of type 2 diabetes significantly increase the likelihood of developing fatty liver disease and its progression to NASH. Studies show that a large percentage of individuals with type 2 diabetes also have some form of fatty liver disease, and a substantial portion of those will have NASH. The interplay between obesity, insulin resistance, and type 2 diabetes creates a highly conducive environment for the development and progression of this severe liver condition. Addressing these core metabolic issues is often the first and most effective step in managing or preventing NASH.
Metabolic Syndrome: A Cluster of Risks
Beyond individual factors, NASH is strongly associated with metabolic syndrome, which is a mix of conditions that, when occurring together, significantly increase a person's risk of heart disease, stroke, and type 2 diabetes. This cluster typically includes:
- Large waistline (abdominal obesity)
- High blood pressure (hypertension)
- High blood sugar (insulin resistance or pre-diabetes/diabetes)
- High triglyceride levels
- Low HDL ("good") cholesterol levels
Having three or more of these conditions dramatically elevates the risk of developing NASH. The components of metabolic syndrome collectively contribute to systemic inflammation and insulin resistance, creating the perfect storm for fat accumulation and subsequent inflammation and damage in the liver. It's a clear indication that NASH is not just a liver problem, but a systemic metabolic disorder with profound implications for overall health. Therefore, managing metabolic syndrome through lifestyle changes and, if necessary, medication, is a critical strategy in preventing or slowing the progression of NASH.
Diagnosing NASH: Beyond the Initial Suspicions
Given the silent nature of NASH, diagnosis can be challenging and often requires a multi-faceted approach. Initial suspicion may arise from routine blood tests showing elevated liver enzymes, or from imaging studies like ultrasound, CT scans, or MRI that detect fat in the liver. While these tests can indicate the presence of fatty liver disease, they cannot definitively distinguish between simple steatosis and the more severe inflammatory form, NASH. This distinction is crucial because it dictates the urgency and type of management required.
To move beyond initial suspicions, doctors may employ more advanced non-invasive tests, such as transient elastography (e.g., FibroScan) or magnetic resonance elastography (MRE). These technologies can assess liver stiffness, which is an indicator of fibrosis. While valuable for identifying individuals with significant scarring, even these tests cannot definitively confirm the presence of inflammation and hepatocyte damage that characterize NASH. They serve as excellent screening tools to identify patients who may need further, more definitive evaluation.
The Crucial Role of Liver Biopsy
Despite advancements in non-invasive diagnostics, the gold standard for diagnosing NASH remains the liver biopsy. This procedure involves taking a small tissue sample from the liver, which is then examined under a microscope by a pathologist. Nash is diagnosed when examination of the tissue with a microscope shows fat along with inflammation and damage to liver cells. This microscopic analysis allows for the precise identification of key features: steatosis (fat), inflammation, ballooning degeneration (damaged liver cells), and the degree of fibrosis (scarring).
The biopsy is critical because it provides a definitive answer regarding the presence and severity of inflammation and damage. If the tissue shows fat without inflammation, it indicates simple steatosis (now MASLD), which has a different prognosis and management approach. Conversely, the presence of inflammation and damage confirms NASH (now MASH), indicating a higher risk of progression and necessitating more aggressive management strategies. While it is an invasive procedure, the liver biopsy offers invaluable information that guides treatment decisions and provides a clear picture of the liver's health, making it an indispensable tool in the accurate diagnosis and staging of NASH.
Managing NASH: Lifestyle as the First Line of Defense
Currently, there is no single FDA-approved medication specifically for NASH. This places a significant emphasis on lifestyle modifications as the cornerstone of treatment. The good news is that for many individuals, proactive changes can effectively halt the progression of NASH and, in some cases, even reverse liver damage. This approach is rooted in addressing the underlying metabolic dysfunctions that drive the disease, offering a powerful pathway to improved liver health and overall well-being.
The first line of treatment for MASLD and MASH (formerly NASH) is weight loss through a combination of choosing healthy foods and increasing physical activity. This isn't just about shedding pounds; it's about improving metabolic health, reducing insulin resistance, and decreasing inflammation throughout the body, especially in the liver. Even a modest weight loss of 5-7% of body weight can significantly improve liver enzyme levels and reduce liver fat, while a loss of 7-10% or more has been shown to reduce inflammation and even reverse fibrosis in some cases.
The Power of Weight Loss and Healthy Choices
Achieving sustainable weight loss and adopting a healthier lifestyle involves a multi-pronged approach:
- Dietary Changes: Focusing on a balanced diet rich in fruits, vegetables, whole grains, and lean proteins is crucial. Limiting intake of processed foods, sugary drinks, saturated and trans fats, and excessive refined carbohydrates is particularly important. A Mediterranean-style diet, known for its anti-inflammatory properties and emphasis on whole foods, is often recommended. Portion control also plays a vital role in managing caloric intake.
- Regular Physical Activity: Engaging in at least 150 minutes of moderate-intensity aerobic exercise per week, combined with strength training, can significantly improve insulin sensitivity, reduce liver fat, and contribute to weight loss. Exercise doesn't just burn calories; it also improves metabolic function independently of weight loss.
- Avoiding Alcohol: While NASH is "nonalcoholic," consuming alcohol can further damage an already compromised liver, accelerating disease progression. Complete abstinence from alcohol is often recommended for individuals with NASH.
- Managing Co-existing Conditions: Effectively controlling conditions like type 2 diabetes, high blood pressure, and high cholesterol is essential, as these factors contribute to the progression of NASH. This may involve medication in addition to lifestyle changes.
The commitment to these lifestyle changes requires patience and perseverance, but the potential rewards – a healthier liver and a reduced risk of severe complications – are immense. Working with healthcare professionals, including dietitians and exercise specialists, can provide personalized guidance and support on this transformative journey.
NASH in Different Age Groups: Children and Adults
While NASH was once primarily considered an adult disease, its prevalence in children and adults is a growing concern, reflecting the global rise in childhood obesity and metabolic syndrome. Discover the prevalence in children and adults, highlighting the alarming trend of this severe liver condition affecting younger populations.
In adults, NASH is most commonly diagnosed in middle-aged individuals, often those over 40 or 50, particularly if they have long-standing risk factors like obesity, type 2 diabetes, or metabolic syndrome. The cumulative effect of years of unhealthy lifestyle choices and metabolic imbalances often manifests in liver damage during these decades. The prevalence in the adult population is substantial and continues to climb, making it one of the leading causes of chronic liver disease and liver transplants worldwide.
However, the most concerning trend is the increasing incidence of NASH in children and adolescents. Pediatric NASH is rapidly becoming the most common cause of chronic liver disease in children in Western countries. This alarming rise is directly linked to the epidemic of childhood obesity and the earlier onset of type 2 diabetes in younger individuals. Children with NASH often present with similar risk factors as adults, including central obesity, insulin resistance, and dyslipidemia. The implications of childhood NASH are particularly dire because these young patients have a longer potential lifespan during which the disease can progress to advanced stages, potentially leading to cirrhosis and liver failure at a much younger age than traditionally observed in adults. Early detection and aggressive lifestyle interventions are even more critical in pediatric populations to prevent a lifetime of liver complications.
The presence of NASH across all age groups underscores its systemic nature and the need for public health strategies that address the root causes of metabolic dysfunction. For both children and adults, understanding the risk factors and pursuing timely medical evaluation are crucial steps in combating the growing burden of this silent yet severe liver disease.
Looking Ahead: Research, Treatments, and Hope for NASH Patients
The global health community recognizes the significant and growing burden of NASH, spurring intensive research efforts to better understand its mechanisms and develop effective pharmacological treatments. While lifestyle modifications remain the cornerstone of management, the quest for targeted therapies is robust, offering substantial hope for patients, particularly those with advanced disease where lifestyle changes alone may not be sufficient to halt progression or reverse damage.
Numerous pharmaceutical companies and academic institutions are actively engaged in clinical trials, investigating a wide array of potential drugs. These investigational therapies target different aspects of NASH pathology, including reducing liver fat, decreasing inflammation, improving insulin sensitivity, and inhibiting fibrosis. Some drugs aim to modulate specific metabolic pathways, while others focus on anti-inflammatory or anti-fibrotic effects. The scientific community is optimistic that several promising candidates are in late-stage development, with the potential to gain regulatory approval in the coming years. This is a rapidly evolving field, with new insights and potential treatments emerging regularly, offering a beacon of hope for those living with NASH.
Beyond drug development, research is also focused on refining non-invasive diagnostic tools to reduce the reliance on liver biopsy, identifying biomarkers for early detection and disease progression, and understanding the genetic and environmental factors that contribute to NASH susceptibility. The goal is to move towards a future where NASH can be diagnosed earlier, managed more effectively with personalized treatment plans, and ultimately, prevented from progressing to end-stage liver disease.
For individuals currently living with NASH, staying informed about research advancements and maintaining close communication with their healthcare providers is vital. While awaiting new pharmacological breakthroughs, adhering to recommended lifestyle changes remains the most powerful tool in managing the disease. The collective efforts of researchers, clinicians, and patients worldwide are paving the way for a future where the severe impact of NASH is significantly mitigated, offering renewed hope for liver health and overall well-being. This article has been medically reviewed by experts, ensuring the information presented is accurate and up-to-date, reflecting the latest understanding in the field.
Conclusion
NASH, or Nonalcoholic Steatohepatitis, represents a critical and often silent threat to liver health, evolving from simple fatty liver to a severe inflammatory condition that can lead to cirrhosis and liver failure. Its strong links to metabolic syndrome, obesity, and type 2 diabetes underscore the importance of addressing systemic health imbalances. While the diagnosis can be challenging, often requiring a liver biopsy, the primary line of defense remains proactive lifestyle changes, particularly weight loss through healthy eating and regular exercise. The growing prevalence of NASH in both adults and children highlights the urgent need for greater awareness and early intervention.
As research continues to advance, offering promising new treatments on the horizon, the power of informed choices remains paramount. Protecting your liver is an investment in your overall health and future. We encourage you to discuss any concerns about liver health with your doctor, share this vital information with your loved ones, and explore other related articles on our site to deepen your understanding of metabolic health. Your proactive steps today can make a profound difference in preventing the severe consequences of NASH.

Research Tools for Fatty Liver Diseases | Cayman Chemical

1955 Nash Ambassador Super | Classic Cars & Used Cars For Sale in Tampa, FL
Frontiers | Pathophysiology of NAFLD and NASH in Experimental Models